Treating Liver Disease: A Look at the Underlying AI Model for Early Detection
At Lucem Health, we’re creating the future of healthcare through the power of clinical Artificial Intelligence (AI), and one new effort focuses on the early detection of metabolic-associated liver diseases. This solution, Reveal for Liver Disease, expands our commitment to leveraging AI to improve patient outcomes by making proactive care easier to deliver to patients who need it the most.
Here, we explore the intricacies of building our underlying AI model for Reveal for Liver Disease. We explain its development, functionality, and the impact it promises for healthcare providers and patients alike.
The Challenge at Hand
Metabolic-associated liver disease (MASLD) and metabolic dysfunction-associated steatohepatitis (MASH), previously known as NAFLD, are increasingly prevalent conditions that often go undiagnosed due to their subtle onset and the limitations of current diagnostic methods. Traditional diagnostic tools either lack the specificity needed or are too invasive and costly for widespread screening. This gap in early detection hampers effective treatment and management of liver disease, underscoring the urgent need for innovation in this space.
Enter Reveal: A Groundbreaking AI Solution
Reveal for Liver Disease is our answer to the challenges plaguing early MASLD/MASH detection. It’s an AI-enabled solution designed to sift through patients’ electronic health records (EHRs) to identify individuals at higher statistical risk of having undiagnosed MASLD or MASH. By analyzing a comprehensive array of data points, including demographic, laboratory, medication, and comorbidity information, Reveal assigns a risk score to each patient. Those exceeding a predefined threshold are flagged for further non-invasive screening, streamlining the process of identifying individuals who merit timely attention.
The Science Behind Reveal
Before building our Reveal solution, we conducted a meticulous review of existing literature and studies on machine learning applications in liver disease detection. Notably, research by McTeer et al. [1], Docherty et al. [2], Chen et al. [3], Chang et al. [4], and Njei et al. [5] demonstrated the potential of machine learning models to outperform traditional biomarkers like FIB-4, NFS or APRI in identifying stages of MASLD and related cirrhosis. Lucem Health’s AI model builds upon the findings from previous research studies, incorporating a superset of features totaling 155 distinct data elements, and explores a variety of machine learning architectures, including advanced learning frameworks like recurrent neural networks and transformer networks.
Our approach is comprehensive, involving training and validation experiments across a large, geographically diverse dataset from thirteen healthcare providers in the US, spanning 14 million patient records across 442 million encounters. This ensures that Reveal is not only based on the most current research but also fine-tuned to perform in real-world settings.
We are currently enrolling pilot sites for a prospective deployment to validate these projections. Get in touch if you would like to learn more about early detection to aid in treating liver disease.
Outperforming Traditional Methods
One traditional method for evaluating liver fibrosis risk is the Fibrosis-4 Index (FIB-4). Despite its widespread use, FIB-4 has limitations, particularly in its ability to differentiate risk for MASLD or MASH. A recent publication by Chang et al. presents an analysis of FIB-4’s effectiveness in identifying MASLD patients with fibrosis (as determined by a liver stiffness measurement exceeding 8kPa and a cardiometabolic condition). Dr. Mazen Noureddin, one of the study’s investigators, cautioned against using FIB-4 for MASLD risk identification:
“Previous studies have shown FIB-4 to have low accuracy for screening liver fibrosis, especially among obese and diabetic patients,” the investigators wrote. “Thus, there is a concern that classifying patients with FIB-4 can lead to misclassification and missed diagnosis.”
In their paper, the investigators analyzed five thousand patients with available liver stiffness results from the National Health and Nutrition Examination Survey (NHANES) dataset. They found that FIB-4 demonstrated a sensitivity of 33% and a specificity of 75% in identifying patients with MASLD and fibrosis. Furthermore, since significant fibrosis is not anticipated during the initial stages of MASLD, FIB-4’s potential to facilitate early diagnosis is further compromised. [6]
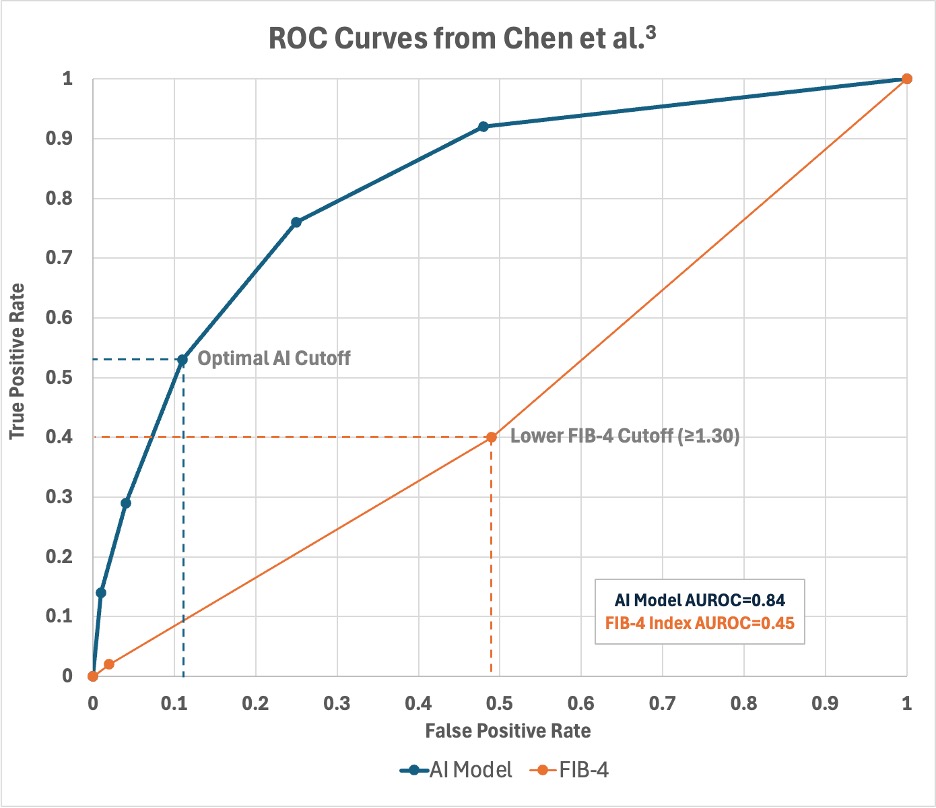
Reveal aims to overcome these limitations by introducing a more precise and efficient method for identifying patients at higher statistical risk for metabolic-associated liver disease. We anticipate that our AI-driven solution will demonstrate significantly greater effectiveness compared to FIB-4. Chen et al.’s study demonstrated that an AI model can achieve a sensitivity of 53% and specificity of 89% (AUROC=0.84), outperforming FIB-4, which only managed a sensitivity of 40% and specificity of 51% (AUROC=0.45) using the lower risk score threshold. [3]
Real-world Impact and Implementation
The implementation of Reveal in clinical settings offers a transformative approach to managing and ultimately treating liver disease. By enabling early detection and triage of high-risk patients, healthcare providers can prioritize care and allocate their clinical resources more effectively. This not only has the potential to improve patient outcomes but also to reduce the overall burden on healthcare systems by streamlining the diagnostic process and reducing unnecessary testing.
Ethical Considerations and Future Directions
As we advance in our journey with Reveal, ethical considerations and patient safety remain at the forefront of our development process. We are committed to transparency and rigorous validation to ensure that our AI recommendations are both trustworthy and understandable to healthcare providers.
Looking ahead, Lucem Health is dedicated to continuous innovation, with plans to expand the capabilities of our AI technology to address a broader range of diseases. Our vision is to harness the full potential of AI in revolutionizing healthcare diagnostics and treatment, improving the lives of patients worldwide.
Conclusion
Reveal for Liver Disease represents a significant leap forward in the early detection of MASLD and MASH. By combining cutting-edge AI with a deep understanding of the challenges in liver disease diagnosis, Lucem Health is creating a new approach to accelerate treatment for patients who need it. We invite healthcare providers to join us in evaluating this innovative solution. We seek a future where liver disease can be detected early, managed effectively, and no longer poses a barrier to a healthy life.
References
- McTeer M, Applegate D, Mesenbrink P, Ratziu V, Schattenberg JM, Bugianesi E, Geier A, Romero Gomez M, Dufour JF, Ekstedt M, Francque S, Yki-Jarvinen H, Allison M, Valenti L, Miele L, Pavlides M, Cobbold J, Papatheodoridis G, Holleboom AG, Tiniakos D, Brass C, Anstee QM, Missier P; LITMUS Consortium investigators. Machine learning approaches to enhance diagnosis and staging of patients with MASLD using routinely available clinical information. PLoS One. 2024 Feb 29;19(2):e0299487. doi: 10.1371/journal.pone.0299487. PMID: 38421999; PMCID: PMC10903803.
- Docherty M, Regnier SA, Capkun G, Balp MM, Ye Q, Janssens N, Tietz A, Löffler J, Cai J, Pedrosa MC, Schattenberg JM. Development of a novel machine learning model to predict presence of nonalcoholic steatohepatitis. J Am Med Inform Assoc. 2021 Jun 12;28(6):1235-1241. doi: 10.1093/jamia/ocab003. PMID: 33684933; PMCID: PMC8200272.
- Chen R, Petrazzini BO, Nadkarni G, Rocheleau G, Bansal M, Do R. Machine Learning Enables Single-Score Assessment of MASLD Presence and Severity. medRxiv [Preprint]. 2023 Oct 25:2023.10.24.23297423. doi: 10.1101/2023.10.24.23297423. PMID: 37961657; PMCID: PMC10635186.
- Chang D, Truong E, Mena EA, Pacheco F, Wong M, Guindi M, Todo TT, Noureddin N, Ayoub W, Yang JD, Kim IK, Kohli A, Alkhouri N, Harrison S, Noureddin M. Machine learning models are superior to noninvasive tests in identifying clinically significant stages of NAFLD and NAFLD-related cirrhosis. Hepatology. 2023 Feb 1;77(2):546-557. doi: 10.1002/hep.32655. Epub 2022 Aug 9. PMID: 35809234.
- Njei B, Osta E, Njei N, Al-Ajlouni YA, Lim JK. An explainable machine learning model for prediction of high-risk nonalcoholic steatohepatitis. Sci Rep. 2024 Apr 13;14(1):8589. doi: 10.1038/s41598-024-59183-4. PMID: 38615137; PMCID: PMC11016071.
- Chang M, Chang D, Kodali S, Harrison SA, Ghobrial M, Alkhouri N, Noureddin M. Degree of Discordance Between FIB-4 and Transient Elastography: An Application of Current Guidelines on General Population Cohort. Clin Gastroenterol Hepatol. 2024 Jul;22(7):1453-1461.e2. doi: 10.1016/j.cgh.2024.02.008. Epub 2024 Feb 29. PMID: 38428706.