The Economics of AFib
Atrial fibrillation (AFib) is a common and serious heart rhythm disorder that affects millions of Americans. It is also a major risk factor for stroke, as it can cause blood clots to form in the heart and travel to the brain. Studies show that AFib-related strokes are more severe and have higher morbidity and mortality rates than strokes caused by other factors.
However, AFib is not always charted on patient records. Many patients are asymptomatic or have intermittent episodes that are not captured by standard ECG tests. Some studies have shown that ECGs are misread or misinterpreted by clinicians at higher rates than one may expect. As a result, less than 80% of AFib cases are correctly diagnosed, and many patients remain unaware of their stroke risk and do not receive appropriate preventive care. [1]
Looking at The Economics of AFib-Related Stroke
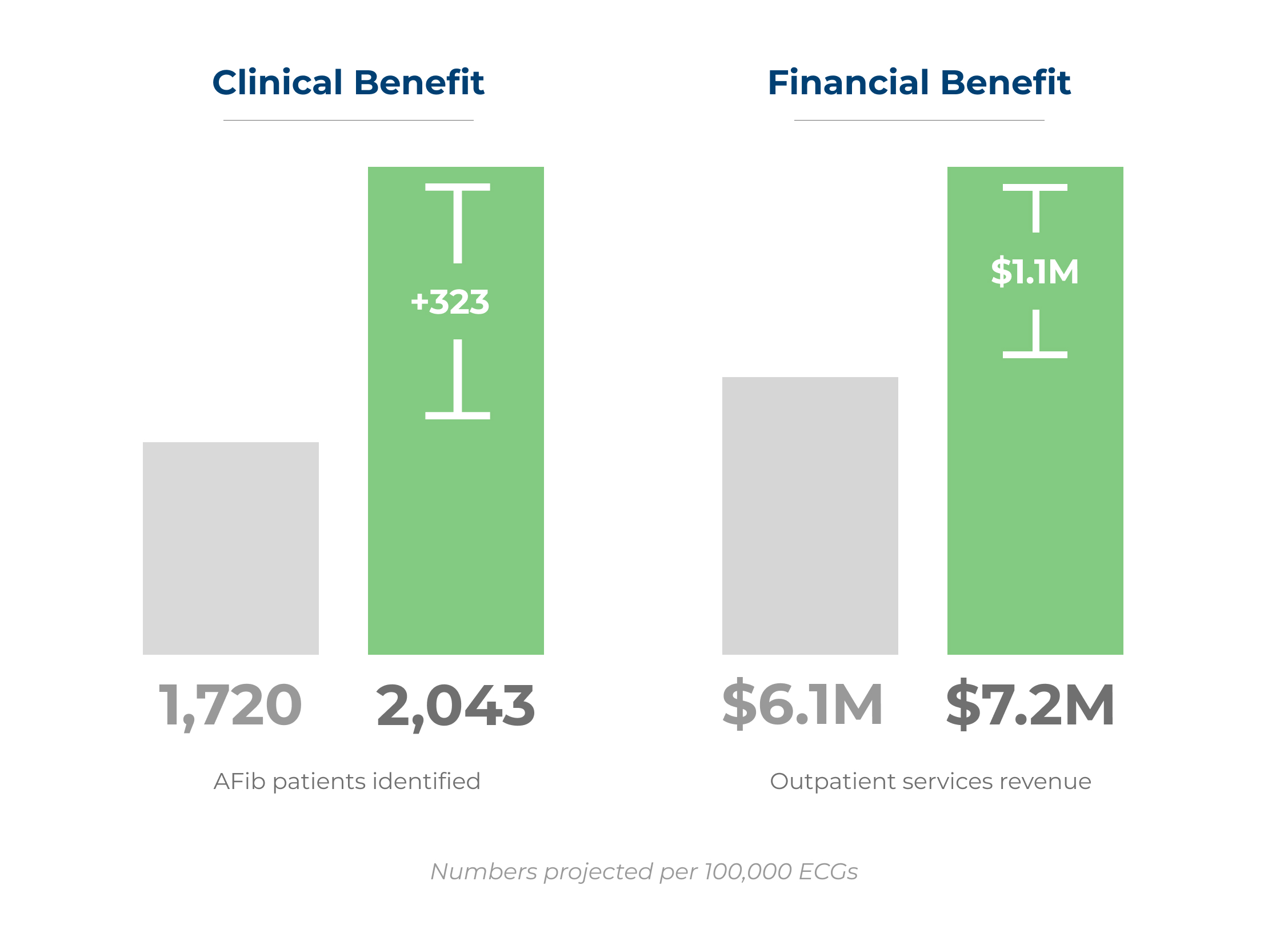
Imagine you could capture most of the patients with uncharged AFib. Based on our health economics analysis, a mid-size provider that performs around 100,000 ECGs per year can expect to identify an additional 181 patients with AFib and high stroke risk. This would translate into a net revenue increase of $1.1 million, over $11.50 per ECG analyzed, from the above-mentioned outpatient services.
How Would This Work?
Automated ECG analysis can help you identify more patients with AFib. Combine these ECG analysis with the patient’s CHA2DS2-VASc score for stroke risk and HAS-BLED score for bleeding risk, and providers will find patients that can benefit most from stroke prevention care and benefit from a roadmap for appropriate clinical action.
By improving your AFib diagnostic rate and funneling more patients into the stroke prevention care pathways, you improve patient outcomes and increase your outpatient services revenue. Examples include:
- Catheter ablation procedures: A minimally invasive procedure that uses radiofrequency energy or cryotherapy to destroy the abnormal heart tissue that causes AFib. It can reduce or eliminate the need for long-term medication and lower the risk of stroke.
- Holter monitoring: A portable device that records the heart’s electrical activity for 24 to 48 hours. It can detect intermittent or paroxysmal AFib that may not be captured by a standard ECG.
- Mobile cardiac telemetry: A wireless device that continuously monitors the heart’s electrical activity and transmits the data to a remote center for analysis. It can detect AFib episodes that may occur over a longer time and alert the clinician for timely intervention.
- Implantable continuous monitors: A small device that is inserted under the skin of the chest and records the heart’s electrical activity for up to three years. It can detect AFib episodes that may be asymptomatic or infrequent and store the data for later retrieval.
- Atrial appendage closure devices: These devices work by blocking off the left atrial appendage, a common site for clot development in AFib, reducing the potential for these clots to cause harm, such as strokes.
- Cardiology clinic visits: A regular follow-up visit with a cardiologist to monitor the patient’s condition, adjust medications, and provide education and counseling.
Wrapping Up
There are even more AFib treatment options, which you can read about here. The bottom line is that identifying patients with uncharted AFib and higher stroke risk need proactive intervention to have the best health outcomes – and that intervention also can support the provider’s bottom line.
You can also check out our AFib white paper, which goes into more detail on all of this and more, here.