Really… Billboards?
Heading Back To the 1980’s
If you’ve driven around a major U.S. city over the last year at all, you’ve probably seen billboards with cheeky messages along the lines of, “if you remember the days of 8-tracks and people could smoke in Pizza Hut, you should get screened for lung cancer.”
Image Source: Michelle Liuzzo/Genentech. All rights reserved.
It’s a clever campaign, but in an era where our wrists vibrate with notifications and our phones are less about calling and more for running our daily lives, the sight of a billboard urging us to screen our lungs feels almost quaint.
Only 6.5% of eligible adults undergo lung cancer screening each year. So while billboards have their place—excellent for promoting burgers or indicating how far the next rest stop is — but with lung cancer remaining the number one cause of cancer deaths in the U.S., we have to ask ourselves: Are billboards and traditional public awareness campaigns really the best we can do against pervasive diseases?
A Wake-Up Call From Katie Couric
Looking back to the late 1990s, Katie Couric’s first husband, Jay Monahan, was diagnosed with colorectal cancer and subsequently passed away from the disease. It was a tragic, high-profile reminder of the risks associated with the disease, even prompting Couric to have an on-air colonoscopy on the TODAY Show in 2000. [1]
Despite the increased awareness from these types of events and the push for screenings for decades, colorectal cancer remains a challenge to detect and diagnose. One-third of age-eligible adults still are overdue for standard screening. [2] Coupled with a declining number of gastroenterologists, this leaves provider organizations today facing an uphill battle to get patients in for screening and ultimately prevent more colorectal cancer cases.
The Diabetes Dilemma
Diabetes, particularly type 2 diabetes, remains a massive public health crisis in the U.S., despite the attention and resources dedicated to its prevention and treatment.
In 2021, approximately 38.4 million Americans had diabetes, with type 2 diabetes making up about 90-95% of these cases. The prevalence of type 2 diabetes has been steadily increasing, with more than 1.2 million new cases diagnosed each year. The financial burden is equally staggering, with the total estimated cost of diagnosed diabetes reaching $412.9 billion in 2022. [3]
Recent developments in drugs, such as Ozempic and Wegovy, which contain the active ingredient semaglutide, are changing the way we treat and manage diabetes. Semaglutide works by mimicking the actions of a naturally occurring hormone called GLP-1, which is released in the gut after eating. GLP-1 helps regulate blood sugar levels by prompting the body to produce more insulin and has effects on the appetite.
In addition to GLP-1 receptor agonists, other innovative weight control treatments, like Setmelanotide (IMCIVREE), which targets rare genetic disorders related to obesity, and naltrexone-bupropion (Contrave), which combines an opioid antagonist and an antidepressant to reduce appetite and control cravings, are gaining traction for their potential to effectively address obesity and metabolic diseases.
These new drugs have been dominating news cycles and social media discourse in much of 2024 – stories of celebrities and everyday people alike seeing great outcomes. Real change is happening, but in conjunction with this increased attention, we must capitalize on finding more ways of identifying undiagnosed prediabetic and diabetic patients in order to actually get them on these new treatment pathways.
Smart Watches & Wearables
Chances are, many of you reading this have a smartwatch on your wrist. And as you know, many smartwatches are capable of detecting atrial fibrillation (AFib), a condition that, if left unchecked, can lead to serious complications like stroke. These watches have shown to be pretty accurate and help put more heart health information directly back into the hands of consumers. [4] It’s a win-win for providers and patients alike, because 24/7 (minus when you charge your watch) you essentially have a real-time monitor checking for signs of heart issues. You still have to go to the doctor to get a diagnosis if you get an alert on your watch, but it is a monumental step in the right direction.
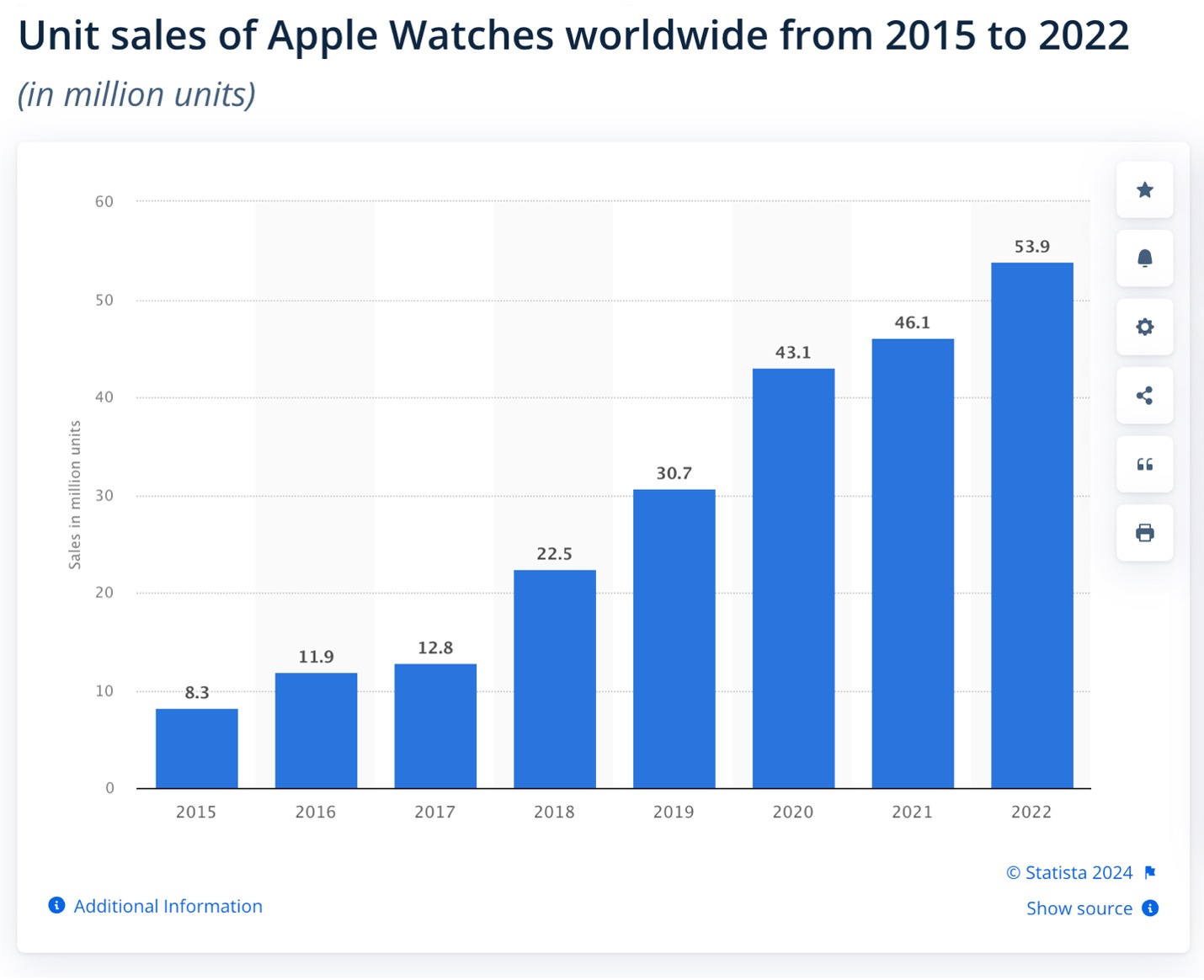
In the last 5 or so years, this technological advancement has certainly shifted public attention toward the risks of AFib and general heart health. [5] While we cannot necessarily link improved public awareness of heart conditions from wearables, the steady increase in Apple Watch sales year-over-year suggest that more and more consumers are aware of – or will learn about — the heart measurement functionality these watches feature.
This sales growth and awareness, however, does not address the pretty large elephant in the room: about 20% of AFib cases still undocumented in clinical practice. Providers and provider organizations still struggle to proactively treat all AFib cases, opening the door for downstream complications. They often have tens of thousands of screening ECGs on file that require further analysis to detect signs of AFib or Atrial Flutter that may have been missed before—a bit like finding a needle in a haystack.
So What Do We Do?
If all these awareness activities and developments aren’t enough to truly combat these diseases, it begs the question, “What else can make a meaningful impact?”
One compelling answer rests with providers and provider organizations, which manage immense stores of patient data. Providers know the strain that these diseases put on the public. They see it every day. But they need ways to more proactively identify patients in their populations that are at higher risk for these diseases, without overworking already strained care teams or using significant resources in the process.
Technology to Close the Gap
Recent developments in clinical solutions powered by AI show great promise in leveraging existing clinical data to detect patients at higher apparent risk:
- For lung cancer, the number one cause of cancer death in the U.S., one AI model can flag ever-smokers 40-89 years old who have higher statistical risk for lung cancer – improving detection and screening efficiency by about 4x.
- In the case of colorectal cancer, provider organizations can use advanced clinical AI with EHR data, looking far beyond factors like anemia and identifying patterns that humans may not. And in doing so, one model can target colorectal cancer at a rate of 8-10x compared to standard screening.
- For diabetes, using an AI-powered solution to analyze standard EHR data would yield about 5x improvement in identification, compared to standard clinical practice.
- Analyzing existing screening ECGs with predictive analytics helps identify 95% of previously undiagnosed AFib cases. Needle in a haystack no longer. Further, these solutions combine AFib detection with a patient’s EHR data to calculate the widely accepted CHA2DS2-VASc stroke risk score – providing clinicians a comprehensive view of a patient’s AFib-related stroke risk. By getting patients on the right treatment pathways, providers can reduce AFib-related strokes by up to 70%.
These AI solutions create an opportunity for clinicians to detect diseases earlier and improve outcomes before they become expensive and complicated to manage. Providers can deliver higher-value, higher-impact care while patients and their families see improved outcomes. All of this yields fewer unplanned admissions and improved resource utilization, along with reduced care costs and higher outpatient revenues.
Looking Beyond Billboards
To fight against common diseases like lung cancer, colorectal cancer, diabetes, and AFib, we can go far beyond billboards. We can offer provider organizations and their patients compelling new technology for early detection and accelerated treatment. In an age where our watches know more about our health than a billboard ever could, healthcare needs to keep pace.